Create a free profile to get unlimited access to exclusive videos, sweepstakes, and more!
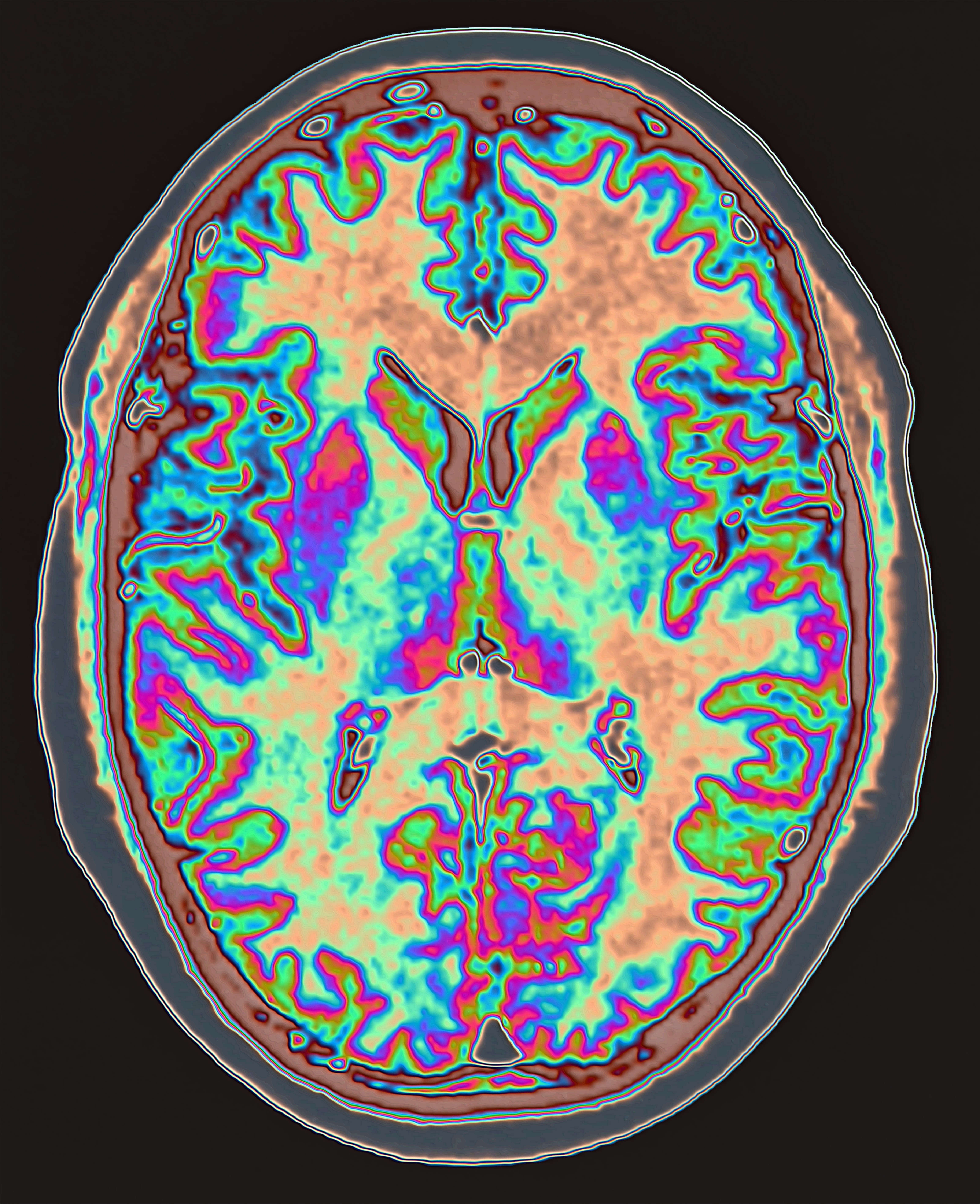
Bespoke brain implants could treat depression and other ailments
In Michael Crichton’s The Terminal Man, protagonist Harold Benson suffers from severe seizures during which he becomes violent. In order to address the seizures, doctors implant electrodes into his brain that are capable of detecting an oncoming seizure and stopping it before it starts.
The violence inherent in Crichton’s tale may have increased the narrative tension in the story, but isn’t indicative of the sorts of real-world patients for whom this technology could be beneficial. In the 50 years since the book’s publication, the idea of crafting a “brain pacemaker” to manipulate brain activity for the benefit of a patient has leapt off the pages of fiction and into reality.
Research conducted by Katherine Scangos, assistant professor in the Department of Psychiatry at the University of California, San Francisco, and colleagues successfully utilized closed-loop deep brain stimulation for the treatment of depression. Their results were published in the journal Nature Medicine.
Unlike traditional treatments like medications which attempt to modulate brain activity across a wide population, closed-loop deep brain stimulation (DBS) is customized to the individual patient’s unique brain activity. The system looks for specific biomarkers correlating to the onset of symptoms and kicks in only when needed, addressing specific incidents as they occur. Open-loop stimulation, another form of DBS, works via a similar process but without the monitoring and incident-targeted stimulation. Where closed-loop DBS initiates based on a specific set of parameters, open-loop stimulates a targeted brain region continuously.
Open-loop DBS has shown promise in treating a number of conditions, including Parkinson’s disease and epilepsy but MDD benefits from a more nuanced approach.
Where the fictional Benson suffered from seizures, the study participant experienced major depression. The ailments differed but the treatment strategy was markedly similar.
First, Scangos and team identified a biomarker present at the onset of symptoms. This is where customization in the process begins. The specific brain activity preceding depressive episodes may vary among individuals and needs to be understood before deep brain stimulation can step in.
The patient, a 36-year-old woman, had experienced Major Depressive Disorder since childhood. Previous treatments, including antidepressants and electroconvulsive therapies, did not substantially improve symptoms, making them a good candidate for deep brain stimulation.
The study began by implanting an array of 10 electrodes into various regions of the brain to monitor and record neural activity over a period of 10 days. Meanwhile, the patient self-reported their symptoms, rating them on a scale.
In order to gather a range of ratings, the patient was asked to complete a number of normal activities like watching a movie or surfing social media. Those ratings were compared to the recorded brain data to identify patterns of activity related to symptomatic states.
Once a biomarker was determined, the temporary electrodes were replaced with a sensory and stimulation device which continually monitors brain activity, looking for the identified biomarker. When and if that marker is detected, the device delivers six seconds of stimulation to the relevant brain regions.
The patient originally presented with a score of 36 on the Montgomery-Asberg Depression Rating Scale (MADRS). After treatment with deep brain stimulation, that score dropped to 14. Several months later, the score had dropped even further, to 10, low enough to be considered remission of symptoms.
Because of the small sample size — one patient — this work does not necessarily predict that the same biomarkers will present in all, or even most, patients with MDD. Likewise, due to the nature of the study, it was not possible to eliminate bias in either the clinicians or the patient. Additional studies with a larger population and control groups will be needed to improve the quality of the data. While less invasive treatment options are preferable for the majority of patients, therapies like closed-loop deep brain stimulation could offer much-needed relief to individuals for whom more traditional therapies are ineffective.
Time will tell if DBS remains effective for this patient long-term, but the preliminary results are promising. Our individual experience of the world and our lives within it are so unique, so personal. There’s something incredibly appealing about neurological therapies that recognize those distinctive traits and treat them accordingly.