Create a free profile to get unlimited access to exclusive videos, sweepstakes, and more!
O really! Transplant organs can now change their blood type to become universal
We're inching closer to one size fits all organs.
Access to a donor organ can be the difference between life and death for thousands of individuals each year. Unfortunately, the demand for organs outstrips the supply. There are currently more than 100,000 people on the transplant waiting list and only about a third of those patients will receive an organ this year. The record for most transplants in a year was set in 2019 with 39,719 total operations.
The remainder of those patients will continue to wait, with 17 people dying each day. Certainly, part of the problem is the total supply of available organs, something doctors and scientists are working to address through novel means like engineering pig organs. Still, many people continue to wait for an organ even while one is available, simply because the organ isn’t a match for their body. Often times a patient with a critical need may be passed over for transplantation, in favor of someone who could stand to wait a little longer, because of tissue compatibility.
A new study carried out by Aizhou Wang from the Latner Thoracic Surgery Research Laboratories and Ajmera Transplant Center at Toronto General Hospital Research Institute, and colleagues, seeks to solve at least a part of this problem. Scientists developed a protocol which changes the blood type of donor organs to O, the universal donor. The results of their preliminary experiments were published in the journal Science Translational Medicine.
“There are other matching requirements. This approach addresses blood type exclusively,” Wang told SYFY WIRE. “It is important to highlight however that blood type matching is currently one of the biggest barriers extending wait times for patients who need a transplant.”
Using two enzymes known as FpGalNAc deacetylase and FpGalactosaminidase, the team was able to take a donor lung and change its blood type from A to O. Blood types are defined by the presence of antigens which don’t play well with one another. The difference between A and O blood types is a matter of a single additional molecule resulting in the A antigen which attaches itself to the surface of red blood cells and organ tissues. The enzymes allowed scientists to remove the antigens, essentially wiping the biological slate clean and preventing unwanted interactions.
“An analogy I like to use is that the enzymes act like magnets and scissors to cut off the blood type A antigens. The magnet side of the enzymes docks on the antigen and the scissor side then chops it off to complete the conversion from type A to type O,” Wang said.
Importantly, because O is the universal donor type, once the organ is converted it becomes compatible with the blood type of any patient.
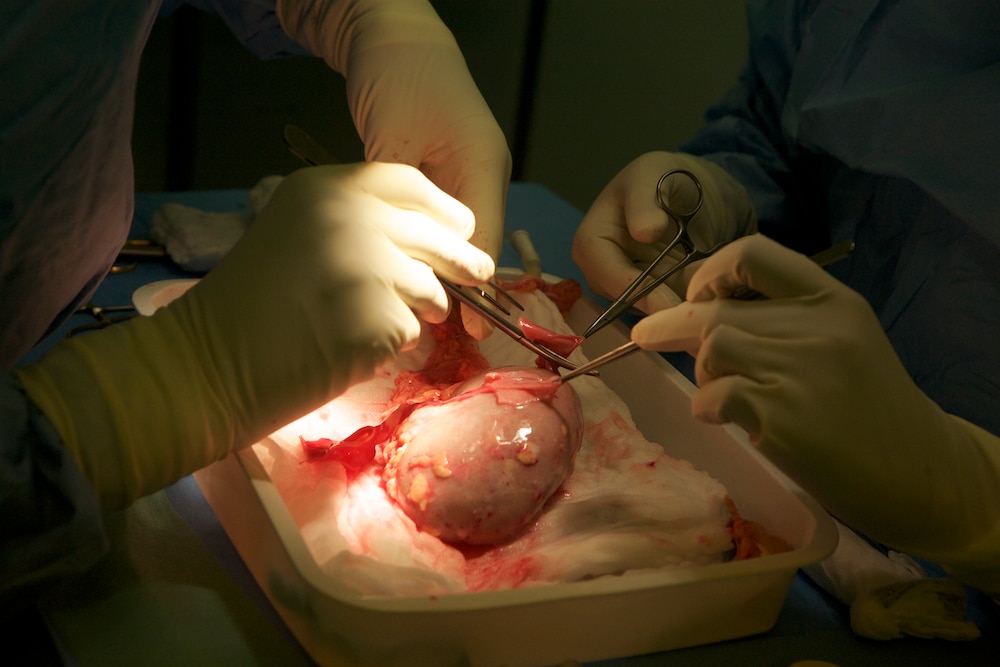
The experiment was carried out ex vivo — outside of the body — as a proof of concept. The team used the Ex Vivo Lung Perfusion System which provides the organs with the necessary nutrients and fluids to remain alive outside of the body and keep them at body temperature.
The donor lungs were then separated into two individual lungs with one acting as the experimental organ and the other a control. One lung was treated with the enzymes to strip away the A antigen, converting it to O blood type while the control organ was not. Both lungs were then filled with O type blood.
In a real-world setting, transplanting an organ with A blood into the body of a patient with O type blood would result in rejection. Type O blood has antibodies which react negatively in the presence of A antigens. That’s precisely what scientists saw in the experiment.
“The results demonstrated that the treated lungs were well tolerated while the untreated ones showed signs of rejection,” Wang said.
More work is needed before this treatment will be ready for use in humans, but it’s a promising first step toward creating universal organs and saving countless lives.