Create a free profile to get unlimited access to exclusive videos, sweepstakes, and more!
Scientists are trying to transform leprosy into a way to regrow livers
Maybe leprosy isn't so bad after all.
Organ failure is one of the most persistent problems in modern medicine. At present, the number of patients waiting for an organ vastly outpaces the availability of those organs, and it’s been that way for a long time. Many people wait years for a lifesaving procedure which may not come in time. Without a workable solution, one could imagine a future like Repo Men, in which malicious corporations lease extended lifespan for a monthly fee. That’s a dystopia worth avoiding, and a recent study published in Cell Reports Medicine suggests we might have found part of the solution.
Professor Anura Rambukkana, the Chair of Regeneration Biology at the University of Edinburgh at the Center for Regenerative Medicine, got his start working with Sir Ian Wilmut, the creator of famed cloned animal, Dolly the sheep. Instead of cloning animals, Professor Rambukkana started his search for nature's regenerative secrets in an unexpected place: mycobacteria, the pathogen responsible for the transmission of leprosy.
“We were looking at skin biopsies from leprosy patients and I noticed that the infected cells were full of bacteria. But if you look at the nucleus, they are even better looking. Brighter. I wondered: how can it be that this terrible disease, it looks like the bacteria isn’t doing anything to the tissues,” Rambukkana told SYFY WIRE.
RELATED: What happened to Viserys' face? 'House of the Dragon' and the science of leprosy
One might expect that a cell bursting with a debilitating infection would show signs of damage, but that wasn’t the case. In fact, the cells had changed for the better. By all accounts, aside from the presence of mycobacteria, the cells appeared to be in their prime. Better than ever. Understanding why that is could be the key to hijacking the bacteria’s machinery for our benefit, and better understanding the mechanisms of our own cells.
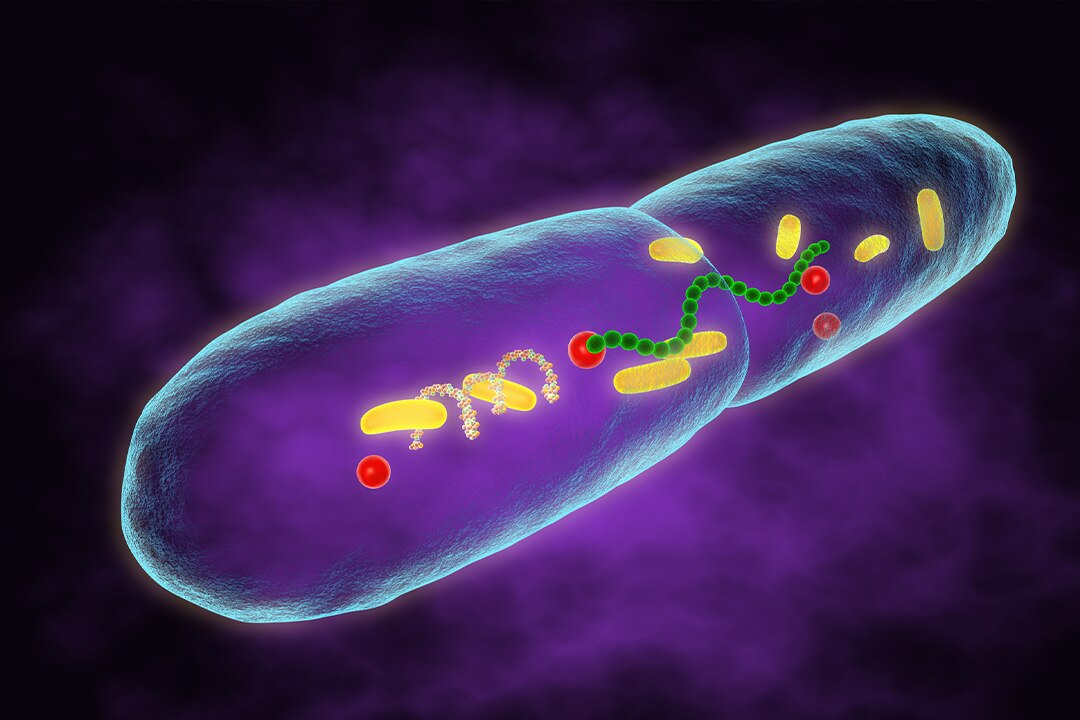
Mycobacteria have one of the longest doubling times of any known bacteria. It takes roughly 14 days between divisions and can take years for an infection to really take hold; that means the bacteria has to hang out in the host cell for a long time. In humans, that means the bacteria hangs out in the nerve cells where immune activity is diminished. Because they have to hide out for so long, and because if they leave the cell they’ll die, it’s in their best interest to keep the cells as happy as possible.
“They take so long to develop inside the cells, and they are totally dependent on the host cells to survive. So, they try to make the cells happy and keep them metabolically active. It makes sense, if you can keep the cells happier, you can get all the goodies from the cell,” Rambukkana said.
In fact, researchers found that one of the most efficient ways to grow nerve cells in a dish is to infect them with leprosy. The bacteria activate a bunch of processes inside the cell which ultimately transform them into what scientists refer to as a stem cell-like state. The question then was whether this phenomenon was an artifact of being in a dish, or if it happened inside a living body as well.
Fortunately for humanity but unfortunately for science, leprosy isn’t a common disease. About 95% of the human population is naturally resistant to infection and the remainder are easily cured with antibiotics. Opportunities for human research are hard to come by, so scientists had to rely on armadillos.
Armadillos are natural carriers of mycobacteria and for the last 40 years, the NIH has funded a facility for growing the pathogen in living armadillos, to support scientific research. In humans, leprosy tends to gather in the extremities or the face, where the temperature is a little lower. Armadillos, however, have a lower core body temperature so the bacteria congregates in the interior, specifically in the liver.
Researchers noticed that infected animals often had larger livers, but it didn’t immediately set off any alarm bells. Organs can sometimes become inflamed when the body has an active infection – anyone who has ever had strep throat with swollen lymph nodes can attest to that – so the phenomenon had a ready explanation. So, Rambukkana sent liver samples, from infected and non-infected armadillos, to a colleague for inspection. The cells were so healthy they couldn’t tell the difference, even when some of the animals had been infected for years. The only signature was that infected livers were up to 50% larger.
Not only were they larger, but they had all of the necessary architecture – blood vessels and bile ducts – to function well. The precise mechanism of this enhanced liver growth isn’t wholly understood, but scientists suggest the bacteria might be taking control of the liver’s innate regenerative pathways to repair damage and construct entirely new tissue.
“Now we want to harness this bacterial ingenuity. If we can translate that… it could be possible to replace the liver transplantation process,” Rambukkana said.
Even in a badly damaged liver, some of the regenerative properties persist. If we can figure out what mycobacteria are doing inside the cells, we might be able to manually improve our own regenerative properties and construct a path toward a future in which doctors don’t repair or replace organs because they repair and replace themselves.


























